The thyroid gland is located in front of your neck just below the voice box (larynx). It makes two hormones thyroxin (T4) and triiodothyronine (T3) that regulates body metabolism. Thyroid hormone production is controlled by another hormone called thyroid-stimulating hormone (TSH), which is released by the pituitary gland, a pea-sized gland located in the brain.

Thyroid disease is a condition that affects the function of the thyroid gland. Thyroid disease results in production of too much or too little of the thyroid hormone. Hyperthyroidism is the disorder that occurs if the thyroid gland produces too much thyroid hormone and may cause the body’s functions to speed up. Hypothyroidism is the disorder that occurs if the thyroid gland produces too little thyroid hormone and may cause the body functions to slow down. Some women have a thyroid disorder that may begin before or during pregnancy or soon after delivery. Thyroid disorders during pregnancy may affect both mother and baby. But with proper treatment, most women with thyroid disorders can have a healthy baby.
Human chorionic gonadotropin (hCG) and Estrogen are the hormones produced during pregnancy that causes increased thyroid hormone levels in your blood. Estrogen increases the amount of thyroid-binding globulin, a protein that is responsible for carrying thyroid hormone. Sometimes the interpretation of tests for thyroid disease is difficult because of the normal changes in the thyroid activity that occurs during pregnancy.
Thyroid hormone is very essential for the normal development of the fetal brain and nervous system. During the first trimester of pregnancy, the foetus is completely dependent on the mother for supply of thyroid hormone. At 10 to 12 weeks, the baby’s thyroid gland begins to produce thyroid hormone on its own. The baby, however, remains dependent on the mother for supply of iodine, which is essential to make the thyroid hormones. During pregnancy women need about 250 micrograms (µg) of iodine per day which can be ensured by use of iodized salt, salt supplemented with iodine.
During pregnancy, the thyroid can slightly increase in size but is not apparent on physical examination by the physician. However, a significantly enlarged gland can be a sign of thyroid disease and should be assessed. The symptoms such as fatigue, higher level of thyroid hormone in the blood, and enlarged thyroid size are common to both pregnancy and thyroid disease can make the diagnosis difficult.
Hyperthyroidism in pregnancy

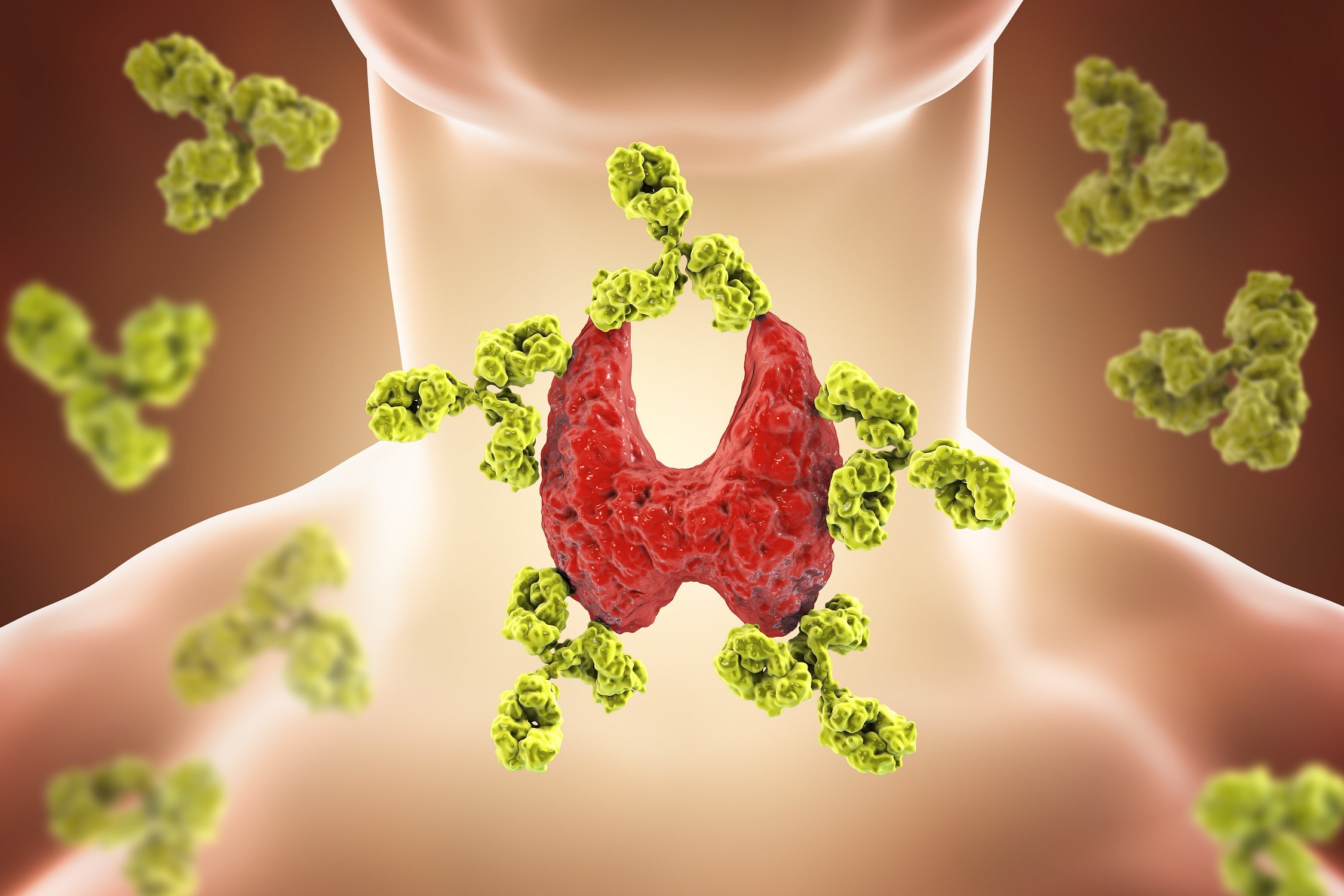
The most common cause of hyperthyroidism during pregnancy is Graves’ disease. Graves’ disease is a condition in which the thyroid gland produces excessive hormones (hyperthyroidism). With Graves’ disease, the immune system makes antibodies that attack the thyroid cells and stimulate the thyroid gland to make more thyroid hormone than your body actually needs. Graves’ disease may be present initially during the first trimester, and in women with pre-existing Graves’ disease, the condition may often improve during the second and third trimester of pregnancy but may worsen during the post-partum period. In addition to other causes very high levels of hCG, seen in severe forms of morning sickness (hyperemesis gravidarum), may cause transient hyperthyroidism that usually resolves by the second half of pregnancy. Uncontrolled hyperthyroidism during pregnancy can cause congestive heart failure, miscarriage, premature birth, low birth weight, thyroid storm (severe hyperthyroidism), and preeclampsia (high blood pressure in late pregnancy).
Hyperthyroidism during pregnancy is treated with anti-thyroid drugs that interfere with thyroid hormone production. These drugs cross the placenta and can impair the baby’s thyroid function and cause hypothyroidism, so the lowest possible dose should be used.
Surgery to remove all or part of the thyroid gland is rarely done and is considered only for women who cannot tolerate anti-thyroid medications. Radioactive iodine therapy is not indicated during pregnancy because it can damage the foetal thyroid gland.
Hypothyroidism in pregnancy
The most common cause of hypothyroidism during pregnancy is the autoimmune disorder known as Hashimoto’s thyroiditis. Hashimoto’s disease is a condition caused by chronic inflammation of the thyroid gland. The resulting inflammation often leads to hypothyroidism, an underactive thyroid gland. With Hashimoto’s disease, the immune system makes antibodies that attack the thyroid cells and damage your thyroid gland making the gland unable to produce the thyroid hormones the body needs. This results in hypothyroidism.
During pregnancy hypothyroidism can occur due to inadequate treatment of pre-existing hypothyroidism or from prior destruction or removal of the thyroid as a treatment for hyperthyroidism. Uncontrolled hypothyroidism during pregnancy, particularly during the first trimester can result in cognitive and developmental abnormalities in the baby.
Hypothyroidism during pregnancy is treated with synthetic thyroxin, which is same as the T4 made by the thyroid gland. In women with known hypothyroidism, the dose is adjusted as needed to maintain normal thyroid function throughout pregnancy.
Postpartum thyroiditis
Postpartum thyroiditis is inflammation of thyroid gland that occurs after childbirth. It occurs within the first year after delivery, usually from one to eight months postpartum. Thyroiditis can cause both hyperthyroidism and hypothyroidism. In postpartum thyroiditis, mild hyperthyroidism occurs first followed by hypothyroidism. For some women, hypothyroidism becomes permanent and requires lifelong treatment with synthetic thyroid hormone. There can be some difficulty in correctly diagnosing postpartum thyroiditis because the symptoms such as exhaustion and moodiness that sometimes develop after delivery may be mistaken for postpartum blues.
Discuss with your doctor if you have symptoms such as fatigue, lethargy, or postpartum depression that remain for a long period of time. In such case you may have developed permanent thyroid condition and may require treatment.
For more details & appointments, please call 800 2344